AI brain cancer prediction is revolutionizing the way healthcare professionals anticipate and manage the treatment of pediatric gliomas, a common type of brain tumor in children. Recent innovations in artificial intelligence have demonstrated a superior capability in cancer recurrence prediction compared to traditional imaging techniques. Leveraging advanced algorithms, AI tools analyze multiple brain scans over time, vastly improving the accuracy of risk assessments. This technology holds promise for optimizing brain tumor treatment by identifying which patients are most susceptible to relapse after surgery. As researchers continue to explore the potential of temporal learning in AI applications, the future of pediatric cancer care looks increasingly hopeful.
The advent of AI-based technologies for predicting brain cancer outcomes represents a significant advancement in medical science. For families grappling with pediatric brain tumors, especially gliomas, the ability to foresee cancer recurrence significantly alters the landscape of treatment and care. Utilizing approaches like temporal learning, these algorithms integrate vast amounts of imaging data over time, offering insights that were previously unattainable. With the potential for enhanced precision in monitoring patients and determining treatment paths, AI in medicine is paving the way for more personalized and effective interventions in pediatric oncology. The implications of these developments extend far beyond the realm of brain tumors, hinting at a broader future where AI enhances diagnostic accuracy across various medical fields.
Understanding Pediatric Glioma and Its Implications
Pediatric gliomas, a form of brain tumor frequently seen in children, represent a complex challenge in oncology due to their varied behavior and potential for recurrence. These tumors can be curable with timely surgical intervention; however, the risk of relapse remains a critical concern for both patients and healthcare providers. The unpredictability of cancer recurrence necessitates a deep understanding of the tumor type and appropriate monitoring strategies. Here, advanced imaging techniques play a vital role, allowing clinicians to assess the effectiveness of treatment and identify any signs of tumor regrowth.
The survival rates for children diagnosed with gliomas have improved significantly in recent decades, but the remnant worry of potential recurrences continues to weigh heavily on families. Thus, clinicians must ensure not only effective treatment but also engaging in continuous monitoring through tools such as MRI scans. Addressing the psychological and physical burden of frequent imaging is essential, which is why the introduction of innovative AI techniques can significantly enhance both patient comfort and treatment outcomes.
The Role of AI in Cancer Recurrence Prediction
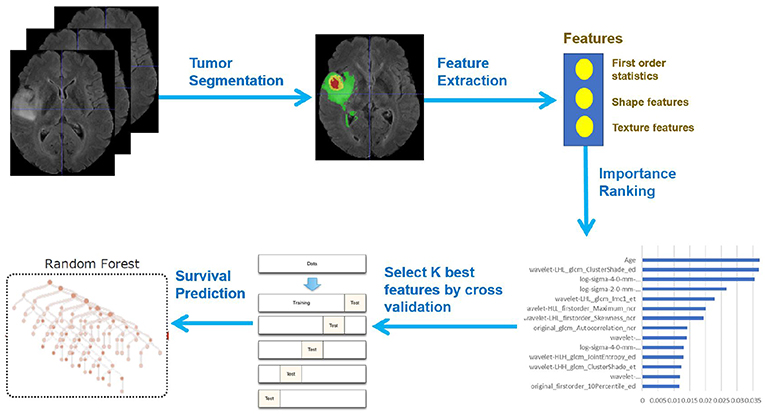
Artificial intelligence (AI) has emerged as a transformative tool in the medical field, especially in predicting cancer recurrence risk in pediatric patients. By analyzing a multitude of brain scans over time, AI technologies offer a nuanced approach compared to traditional methods that rely on single images. This proactive strategy enables clinicians to detect subtle changes in the brain’s condition, refining their ability to forecast potential relapses effectively. As seen in studies focusing on pediatric glioma, the advanced algorithms develop an understanding of typical progression patterns, thus enhancing the predictive accuracy for recurrence.
The recent research conducted by Mass General Brigham illustrates the paradigm shift brought about by AI in oncology. With the use of temporal learning—a methodology that amalgamates learnings from multiple imaging sessions—the AI tool has demonstrated an impressive accuracy rate of 75-89% in predicting glioma recurrence. Such advancements not only support timely and targeted interventions but also enable healthcare providers to tailor follow-up care more effectively, enhancing the quality of life for young patients and their families.
Exploring Temporal Learning in Medical Imaging
Temporal learning represents a significant advancement in AI applications within the domain of medical imaging. Unlike traditional methods where analyses are performed on isolated images, temporal learning focuses on a series of scans taken over several months. This dynamic approach allows the AI to identify patterns and changes that may indicate a potential recurrence of brain tumors post-surgery. By sequencing a patient’s MR scans chronologically, researchers can train the model to detect even the slightest variations, which can be critical in an inpatient setting where timely action is paramount.
The utilization of temporal learning grants a more profound insight into the disease’s progression and has implications beyond pediatric gliomas. This methodology could revolutionize cancer care by offering a model that adapts to various patient scenarios, thus enhancing predictive capabilities. As the medical community continues to understand the implications of temporal learning, it can pave the way for breakthroughs in treatment for numerous other conditions requiring long-term imaging follow-ups.
AI Brain Cancer Prediction: The Future of Pediatric Care
As the capabilities of AI in brain cancer prediction evolve, there lies considerable hope for enhancing the standard of care in pediatric oncology. The AI tool developed by researchers represents a significant leap towards accurately identifying which patients are likely to experience cancer recurrence. By integrating machine learning algorithms with temporal sequencing of brain scans, healthcare providers can make evidence-based decisions tailored to individual patient needs. This development heralds a new era of personalized medicine where AI guides treatment plans based on precise data.
The anticipated integration of AI tools into clinical practice will not only streamline the monitoring process for patients with gliomas but may also foster a more proactive approach to treatment. Prospective clinical trials will be essential in validating these AI techniques, ensuring that they yield benefits in real-world applications. As the healthcare industry increasingly embraces AI in medicine, the potential for improved outcomes and reduced patient burdens in the management of pediatric brain tumors presents a promising future.
Advancements in Brain Tumor Treatment Strategies
The treatment of pediatric brain tumors, particularly gliomas, has saw substantial advancements over recent years. With surgical methods having high success rates, the focus has shifted towards improving post-surgical care and monitoring for potential relapses. AI technologies play a crucial role in refining these treatment strategies, allowing for a custom-tailored approach that takes into account the unique characteristics of each tumor. Enhanced imaging and prediction capabilities mean that patients are less likely to endure unnecessary procedures and imaging, directly reducing the emotional and physical toll on young patients and their families.
Moreover, the incorporation of predictive analytics in treatment regimens opened up avenues for innovative therapies, such as targeted adjuvant treatments for those identified at higher risk of recurrence. Such advancements support not just survival but also quality of life outcomes in pediatric oncology. By continually leveraging emerging technologies like AI, the medical community can ensure that the fight against pediatric brain tumors becomes increasingly effective and compassionate.
Reducing Imaging Frequency with AI Insights
One of the significant impacts of AI in managing pediatric glioma is the potential reduction in the frequency of imaging procedures for low-risk patients. Traditionally, children at risk of tumor recurrence underwent routine MRIs that could lead to increased anxiety and physical strain. However, with the predictive capabilities of the new AI model, healthcare providers can more accurately assess which patients legitimately require frequent monitoring. This shift not only eases the psychological burden on families, but it can also allocate healthcare resources more efficiently, focusing attention where it is genuinely needed.
By stratifying patients effectively—identifying those with a minimal likelihood of recurrence—clinicians can create a more comfortable follow-up plan and potentially direct resources toward high-risk patients who may require closer surveillance. The prospect of reducing imaging frequency allows healthcare providers to strike a balance between thoroughness in care and minimizing the disruption to patients’ lives, ultimately leading to better overall patient satisfaction.
The Importance of Collaboration in Cancer Research
Collaboration among healthcare institutions plays a vital role in advancing research on pediatric cancers like gliomas. The study conducted by Mass General Brigham exemplifies how joint efforts among various hospitals and research centers can pool resources, data, and expertise to tackle complex medical challenges. By gathering an extensive database of MR scans from diverse populations, researchers can enhance the validity of AI training models, enriching the algorithms’ learning experience and improving their predictive capabilities.
These partnerships can significantly expedite the pace of medical innovation, particularly in areas like cancer recurrence prediction. As institutions work together, they can establish standardized practices and share best practices, ultimately fostering an environment of collaboration that yields better treatments and care pathways. This synergistic approach is paramount not only in dealing with pediatric gliomas but across the spectrum of medical research, paving the way for breakthroughs that benefit patients everywhere.
Towards Clinical Trials: Validating AI Predictions
The promising results from studies that incorporate AI for cancer recurrence predictions signify an important step toward clinical trials. Although researchers have established a solid foundation through retrospective analyses and predictions based on longitudinal imaging, the transition to clinical settings remains crucial for obtaining empirical validation. It is through rigorous clinical trials that the safety and effectiveness of these AI models can be confirmed, ensuring that they deliver reliable guidance in practice.
The commitment to explore AI-derived predictions in clinical environments will not only refine treatment protocols for pediatric glioma but also inspire trust in the capabilities of AI in medicine. By collecting prospective data from these trials, researchers can evaluate the tangible benefits of predictive analytics on patient care outcomes, further solidifying the role of AI as a game-changer in oncology and potentially in various other domains of healthcare.
Future Directions in Pediatric Brain Tumor Research
With the ongoing advancements in technology and AI, the future directions in pediatric brain tumor research look incredibly promising. The exploration of machine learning techniques to analyze imaging data represents just the beginning; future research may uncover even more sophisticated algorithms capable of predicting treatment responses and adjustments required based on individual patient needs. These advancements could lead to more personalized and effective treatment plans and ultimately improve survival rates for children diagnosed with brain tumors.
Continuous investment in research applicable to pediatric gliomas and collaboration among various healthcare institutions will be essential for driving future innovations. As the landscape of cancer treatment evolves, with AI at the forefront, the hope is to transition from reactionary treatment approaches to proactive care strategies that focus not only on survival but also on the quality of life for patients and their families.
Frequently Asked Questions
How does AI brain cancer prediction improve outcomes for pediatric glioma patients?
AI brain cancer prediction leverages advanced algorithms to analyze multiple brain scans over time, significantly enhancing the ability to forecast recurrence risks in pediatric glioma patients. This technology surpasses traditional methods by achieving up to 89% accuracy in predicting cancer relapse, ultimately promoting more effective treatment strategies and personalized care.
What role does temporal learning play in AI brain cancer prediction for pediatric gliomas?
Temporal learning is a crucial technique in AI brain cancer prediction, as it enables the model to assess a sequence of brain scans taken over time rather than just single images. This approach helps the AI recognize subtle changes in tumor characteristics, improving the accuracy of recurrence predictions for pediatric gliomas.
Can AI in medicine help reduce anxious follow-ups for children recovering from brain tumors?
Yes, AI in medicine enhances the prediction of cancer recurrence, allowing for a more tailored follow-up strategy. By accurately identifying low-risk pediatric glioma patients, AI brain cancer prediction can reduce unnecessary imaging and related stress, ultimately leading to a more supportive recovery environment.
What is the significance of AI in predicting cancer recurrence for pediatric glioma patients?
The significance of AI in predicting cancer recurrence for pediatric glioma patients lies in its ability to provide early and accurate risk assessments. By employing advanced AI brain cancer prediction techniques, healthcare providers can identify patients who are most at risk of relapse and tailor their treatment plans accordingly.
How does the accuracy of AI brain cancer prediction compare to traditional methods?
AI brain cancer prediction offers a substantial increase in accuracy compared to traditional methods. In the study mentioned, AI models demonstrated accuracy rates of 75-89% in predicting glioma recurrence, while conventional predictions based on single scans were only 50%, highlighting the efficacy of AI in improving patient outcomes.
What future implications do AI tools have for brain tumor treatment in pediatric cases?
AI tools hold promising future implications for brain tumor treatment in pediatric cases, including the potential to optimize treatment strategies. Through enhanced recurrence prediction capabilities, AI brain cancer prediction can guide decisions on when to escalate treatment or reduce follow-up care, ultimately leading to better outcomes for children with gliomas.
| Key Points | Details |
|---|---|
| Use of AI for Prediction | An AI tool has been developed that predicts the risk of relapse in pediatric brain cancer patients more accurately than traditional methods. |
| Study Background | Conducted by researchers from Mass General Brigham and Boston Children’s Hospital, the study utilized nearly 4,000 MR scans from 715 patients. |
| Temporal Learning Technique | The AI employs a technique called temporal learning, which analyzes multiple scans over time rather than individual scans. |
| Accuracy of Predictions | The AI model predicted recurrence with an accuracy of 75-89%, far exceeding the 50% accuracy of single image analysis. |
| Clinical Implications | Research aims to initiate clinical trials to validate the findings and potentially improve care by tailoring follow-ups and treatments. |
Summary
AI brain cancer prediction holds significant promise for enhancing the management of pediatric gliomas. By utilizing advanced AI techniques, researchers have demonstrated a remarkable improvement in predicting cancer recurrence compared to traditional methods. This innovative approach not only alleviates some of the stress associated with frequent imaging for children and their families but also paves the way for enhanced patient care through targeted treatments based on individual risk assessments. As further validation and clinical trials unfold, the potential of AI in advancing brain cancer prediction continues to grow, presenting hope for better outcomes in pediatric oncology.