Pediatric cancer recurrence remains a significant concern for both patients and their families, particularly in the context of brain tumors like pediatric gliomas. Recent advancements in AI predicting cancer have opened new avenues for understanding and mitigating the risk of relapse in young patients. A groundbreaking study revealed that an AI tool leveraging MRI scans pediatric patients over time can predict recurrence with remarkable accuracy, surpassing traditional methods of cancer risk assessment. This innovative approach not only relieves some of the burdens associated with frequent imaging but also provides valuable insights into which patients would benefit from targeted treatments. The potential of temporal learning AI to transform how we approach pediatric cancer recurrence highlights the importance of integrating technology in healthcare for improved outcomes.
The topic of pediatric cancer recurrence, often marked by the challenges of managing childhood malignancies, is increasingly receiving attention in the medical community. Young patients, especially those diagnosed with brain tumors, face a daunting journey where the threat of a relapse looms large. Recent studies have demonstrated that advanced AI technologies can significantly enhance the accuracy of predicting cancer relapses by analyzing multiple medical images over time. Furthermore, methodologies like temporal learning are enabling physicians to better assess cancer risk, ultimately aiming to provide earlier interventions for at-risk patients. As these tools continue to evolve, they promise to redefine how pediatric oncology addresses the complexities of treatment and recovery.
Understanding Pediatric Cancer Recurrence Risks
Pediatric cancer recurrence presents a significant challenge for both patients and their healthcare providers. When a child initially diagnosed with cancer undergoes treatment, such as surgery, there is often a sense of relief. However, the risk of recurrence can loom, particularly with tumors like pediatric gliomas. Research indicates that while many of these tumors can be treated effectively, the likelihood of returning cancer necessitates ongoing vigilance, resulting in prolonged follow-up care and frequent MRI scans.
The complexity of predicting pediatric cancer recurrence highlights the urgent need for more precise risk assessment tools. Traditional methods often rely on a snapshot in time, assessing images from single MRI scans without considering changes over time. This approach can lead to uncertainty and anxiety for families waiting on results. As such, advancements in AI, especially those employing techniques like temporal learning, could revolutionize how we predict and manage the risk of relapse in pediatric cancer patients.
The Role of AI in Predicting Pediatric Cancer Outcomes
Artificial intelligence is changing the landscape of medical imaging, particularly in relation to cancer prediction. The recent study from Mass General Brigham showcases how an AI tool was able to analyze longitudinal MRI scans with greater accuracy than traditional methods, marking a significant advancement in the assessment of pediatric cancer risks. By leveraging data from nearly 4,000 brain scans, the AI model trained with temporal learning techniques was able to identify patterns that indicate potential relapse sooner than previously possible.
This predictive capability is crucial in clinical settings where timely interventions can dramatically alter outcomes. For instance, with a predictive accuracy rate of 75-89%, as opposed to 50% through conventional imaging, the AI model could effectively stratify patients into low- or high-risk categories. This means that healthcare providers can offer personalized treatment plans, potentially reducing unnecessary imaging for those at lower risk while ensuring higher-risk patients receive appropriate follow-up care.
MRI Scans in Pediatric Cancer: A Necessity or Burden?
Magnetic Resonance Imaging (MRI) scans are a fundamental aspect of monitoring pediatric cancer patients post-treatment. They provide crucial insights into the status of the brain and any potential changes that could indicate a recurrence of cancer, particularly for conditions such as pediatric gliomas. However, the frequency of these scans can become a source of stress for both children and their families due to the waiting and uncertainty associated with results.
Innovative AI tools that enhance the predictive accuracy of these scans could not only ease the emotional burden linked to frequent monitoring but also optimize the healthcare process. By understanding how to better utilize MRI data, those in the medical community can tailor their approaches, potentially decreasing the frequency of scans for patients identified as low-risk while maintaining a close watch on those in higher-risk categories, ultimately facilitating a more efficient use of healthcare resources.
The Promise of Temporal Learning in AI for Medical Imaging
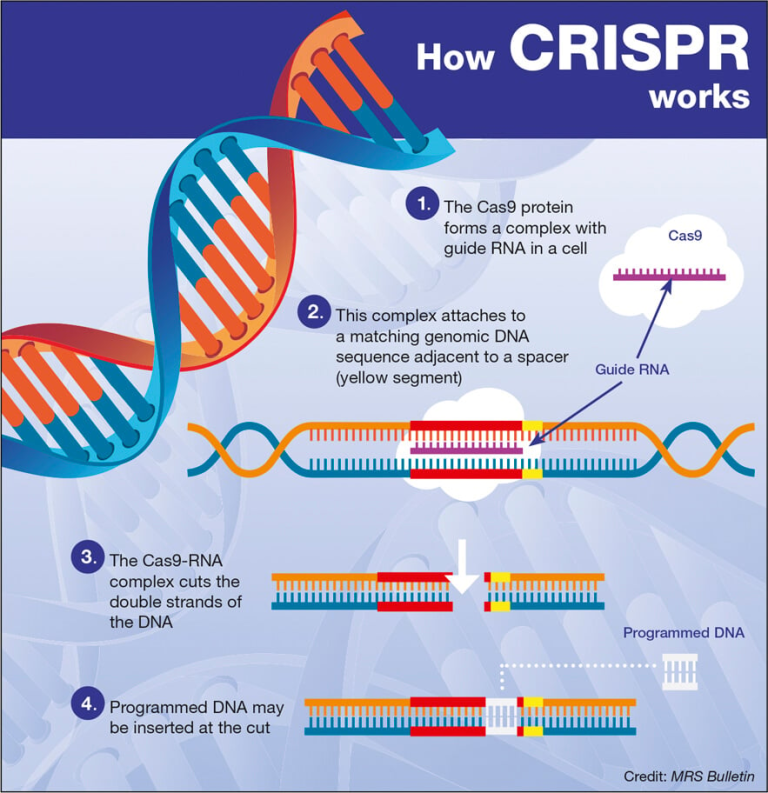
Temporal learning is an exciting new frontier in AI that allows models to analyze sequences of images over time, which is particularly beneficial in the context of pediatric cancer. Unlike traditional AI models that focus exclusively on single MRI scans, temporal learning enables the extraction of trends and subtle changes that could indicate cancer recurrence. This innovative approach is making waves in how we predict patient outcomes and manage follow-up care for children with brain tumors.
In practical terms, the implementation of temporal learning can vastly improve the way clinicians interact with postoperative imaging results. By training AI tools to analyze the progression of patients’ conditions over time, healthcare providers can not only identify those at risk of recurrence more accurately but can also potentially intervene sooner, improving the overall prognosis for many pediatric cancer patients. This focus on longitudinal data analysis is becoming increasingly relevant as we seek to refine cancer risk assessment processes.
Clinical Implications of AI-Driven Risk Assessment
The findings from the recent study open up significant discussions regarding the clinical implications of AI in pediatric oncology. If validated across different healthcare settings, these AI-driven risk assessments could transform routine follow-ups and patient care strategies. Pediatric patients identified at lower risks for recurrence may benefit from a reduced imaging schedule, thus minimizing unnecessary exposure to MRI procedures and lessening emotional strain on families.
Conversely, high-risk patients could be flagged for early intervention strategies, including tailored adjuvant therapies aimed at managing potential relapses effectively. This proactive approach not only aims to improve survival rates but also enhances the quality of life for young patients and their families during a challenging time. The evolution of risk assessment in pediatric cancer showcases the importance of integrating advanced technologies such as AI into standard treatment protocols.
Future Research Directions in Pediatric Cancer AI Applications
As the field of AI in healthcare continues to evolve, it becomes increasingly important to explore the future directions for its application in pediatric oncology. The promising results from recent studies emphasize the need for comprehensive clinical trials to assess the effectiveness of AI-informed predictions on patient outcomes. Researchers are looking to develop larger datasets incorporating diverse populations to enhance the models further and ensure they are applicable across various demographic and clinical settings.
Furthermore, understanding the ethical implications and ensuring that AI systems are transparent and fair in predicting cancer risks is vital. Ongoing collaboration between AI experts, oncologists, and data scientists will facilitate the refinement of these technologies, ultimately aiming to create systems that empower healthcare professionals while providing the best possible outcomes for pediatric cancer patients.
The Emotional Toll of Cancer Monitoring on Families
The journey through pediatric cancer treatment and follow-up care is fraught with emotional challenges for both the child and their family. While the use of MRI scans is necessary for monitoring, the anxiety associated with waiting for results can be overwhelming. Families often bear not only the psychological burden of knowing their child is at risk but also the stress of navigating frequent medical appointments and the uncertainties that come with cancer recurrence.
AI-driven tools in predicting pediatric cancer recurrence aim to alleviate some of these emotional pressures by providing clearer insights into risks, potentially reducing the frequency of imaging for low-risk patients. This innovative approach can allow families to focus on their child’s well-being rather than constantly worrying about recurrence. By incorporating these advanced technologies into pediatric care, we can improve not only clinical outcomes but also enhance the overall experience for families affected by cancer.
AI Predictive Models: Enhancing Treatment Strategies in Pediatric Oncology
The integration of AI predictive models into pediatric oncology signifies a paradigm shift in how treatment strategies are devised. With traditional approaches often reliant on vague prognostic indicators, the precision offered by AI tools allows for a more personalized approach to patient care. This is particularly vital for managing conditions such as pediatric gliomas, where treatment plans can be finely tuned based on individual relapse risk assessments conducted through AI.
As organizations like Mass General Brigham innovate with AI, we can expect treatment plans to become more focused and effective, allowing for interventions that are timely and targeted. This technological leap is integral to advancing pediatric cancer care, as it bridges the gap between clinical research and bedside practice, translating complex data into actionable insights that can significantly alter the trajectory of a young patient’s journey.
Conclusion: The Future of Pediatric Cancer Care with AI
The future of pediatric cancer care looks promising, especially with the advancements in artificial intelligence and machine learning. Innovations like temporal learning and improved imaging techniques are set to redefine standard practices in monitoring and treatment, helping healthcare providers offer better prognostics and care. As we continue to unlock the potential of AI in predicting pediatric cancer recurrence, both clinicians and families can look forward to a more informed and less intimidating path through the challenges posed by cancer.
Continued research and development will be essential in harnessing the full capabilities of AI. By ensuring that these technologies are validated and implemented effectively, we can strive toward personalized medicine that not only enhances survival rates but also improves the overall quality of life for children battling cancer. Embracing these changes holds the key to creating a future where pediatric cancer care is more about hope and less about fear.
Frequently Asked Questions
What is the role of AI in predicting pediatric cancer recurrence, such as in pediatric gliomas?
AI plays a significant role in predicting pediatric cancer recurrence, particularly in pediatric gliomas. Recent studies have shown that AI tools, through advanced techniques such as temporal learning, can analyze multiple MRI scans over time to assess a child’s risk of relapse with high accuracy. This method allows healthcare providers to identify which patients may be at higher risk for recurrence more effectively than traditional methods.
How do MRI scans contribute to understanding cancer recurrence in pediatric patients?
MRI scans are crucial in monitoring pediatric cancer recurrence. They provide detailed imaging of the brain, allowing physicians to track changes over time. In the context of pediatric gliomas, AI-enhanced analysis of these scans can significantly improve the prediction of cancer recurrence, making follow-ups more efficient and less burdensome for patients and their families.
What advancements have been made in cancer risk assessment for pediatric glioma patients?
Advancements in cancer risk assessment for pediatric glioma patients include the use of AI tools that leverage temporal learning. This innovative approach analyzes a series of MRI scans to detect subtle changes that may indicate a risk of recurrence, enhancing the ability to predict which patients might need more intensive monitoring or treatment.
Can AI tools improve the frequency of imaging required for pediatric cancer recurrence monitoring?
Yes, AI tools can potentially improve the frequency of imaging required for monitoring pediatric cancer recurrence. By accurately predicting which patients are at low risk, healthcare providers may reduce unnecessary MRI scans, alleviating the emotional and physical burden on children and their families while still ensuring that those at higher risk receive timely interventions.
What is temporal learning AI and how does it aid in predicting pediatric cancer recurrence?
Temporal learning AI is an advanced technique that trains algorithms to analyze multiple MRI scans taken over time, rather than just single images. This allows the AI to detect subtle changes that might indicate cancer recurrence. In pediatric cancer, particularly gliomas, this method has demonstrated significantly higher accuracy in predicting recurrences compared to traditional single-scan analysis.
What are the potential benefits of AI in managing pediatric cancer recurrence?
The potential benefits of AI in managing pediatric cancer recurrence include improved accuracy in predicting relapse risks, reduced unnecessary imaging for low-risk patients, and the ability to tailor treatment plans more effectively for high-risk patients. This could lead to better outcomes for children facing the challenges of brain tumors like gliomas.
How does AI compare to traditional methods in assessing the risk of pediatric cancer recurrence?
AI has shown to outperform traditional methods in assessing the risk of pediatric cancer recurrence. In studies involving pediatric gliomas, AI tools utilizing temporal learning achieved prediction accuracies of 75-89%, compared to just 50% with conventional approaches. This significant improvement underscores the potential of AI to revolutionize cancer risk assessment in pediatric patients.
What impact could AI-driven predictions have on pediatric glioma survivors?
AI-driven predictions could significantly impact pediatric glioma survivors by allowing for tailored monitoring and treatment strategies. By effectively identifying which survivors are at higher risk of recurrence, healthcare providers can implement preventive measures sooner, ultimately improving long-term health outcomes and reducing the emotional and physical impacts of ongoing monitoring.
| Key Point | Details |
|---|---|
| AI Tool for Recurrence Prediction | AI surpasses traditional methods in predicting cancer relapse in pediatric patients. |
| Use of Temporal Learning | Innovative technique that uses multiple brain scans over time to improve predictions of cancer recurrence. |
| Study Findings | The AI model accurately predicts recurrence with an accuracy of 75-89%, compared to 50% for single scans. |
| Impact on Patient Care | Expected improvements in care by reducing frequent follow-ups for low-risk patients and targeted treatment for high-risk patients. |
| Future Steps | Further validation and launching clinical trials to determine the efficacy of AI in clinical settings. |
Summary
Pediatric cancer recurrence is a critical concern for both families and healthcare providers. Recent advancements, particularly in AI technology, have shown promise in enhancing prediction accuracy for cancer relapse in pediatric patients. By leveraging innovative techniques like temporal learning, researchers are working towards improving care strategies, ultimately aiming to alleviate the emotional and physical burden associated with frequent follow-ups. This progress highlights the potential for AI to transform the management and treatment of pediatric cancers, particularly gliomas.